Shock
Initial Assessment & Management
Hypovolaemic Shock
Step 1
• Stop external bleeding - Go to Catastrophic Haemorrhage
Step 2
• Assess the cause of the hypovolaemic shock:
- haemorrhage (trauma or non-trauma)
- plasma (burns)
- electrolyte solution (diarrhoea and/or vomiting)
Step 3
• Estimate the degree of hypovolaemic shock from the table

Diarrhoea and/or vomiting
• Start fluid resuscitation with 0.9% NaCl (normal saline) or Hartmann’s solution. Refer to
Compendium for specific treatment of infectious causes of D&V.
Consider Sepsis
Related guidelines:
Heat illness
Burns
• Estimate the size of the burn using the Rule of Nines or the Lund and Browder Chart.
Go to Toolbox:
National Early Warning Score (NEWS)
Resource: FMED 1061
Estimate the weight of the patient to the nearest 10kg.
• Estimate the time since the injury to the nearest hour.
• Now use the Burns calculator to determine the fluid requirement. Fluid is
replaced as N/Saline solution only pre-hospital. Once at hospital use
Hartmann’s.
Go to Toolbox:



Advanced Assessment & Management
Fluid replacement strategy in haemorrhagic shock
1. The optimum treatment for haemorrhage is definitive surgical control of
bleeding and volume replacement with blood products.
2. Where blood products and/or surgical facilities are not available, a restrictive
resuscitation strategy should be used for the first hour after injury – aim to
maintain a palpable radial pulse.
3. Give 0.9% NaCl (normal saline) or Hartmann’s solution in 250ml aliquots and
assess response.
4. In patients with hypovolemic shock and a severe head injury, or if the patient
is pregnant or is a child, aggressive management to maintain a strong radial
pulse should be undertaken.
5. When possible to take a formal BP, the target Blood Pressure in these cases
should be a systolic of 110 mmHg.
6. In ALL cases, 1 hour post-injury, aim for a strong radial pulse (systolic of
110mm Hg)
7. Use 1g tranexamic acid as soon as possible in patients with major trauma and
hypotension due to bleeding.
8. If blood products are available, a major haemorrhage protocol should be
utilised.
9. Monitor the effect of volume resuscitation using the pulse rate, pulse
pressure, blood pressure, respiratory rate and hourly urine output.
Resource: NICE trauma guidelines 2019. NICE Pathways - Major Trauma in the PreHospital Setting
Note military guidance differs in that it does not differentiate between blunt and
penetrating trauma.
Intraosseous Access

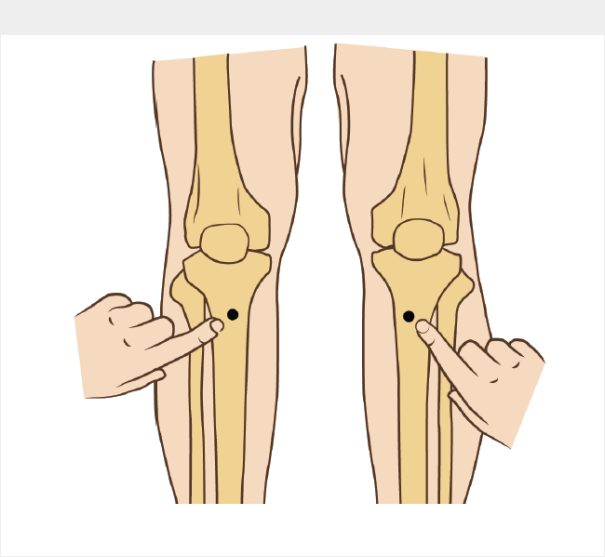
Anterio-medial aspect of the tibial tuberosity:
• Lay patient supine on stretcher
• Extend the leg
• Identify the tibial tuberosity
• Measure approx 3cm down and 2cm medially.
• Use BLUE needle as the first choice
• Ensure needle size is appropriate before drilling
EZ-IO Sites - Humerus
• Lay patient supine on stretcher
• (Patient's) hands over testicles
• Trace clavicle from sternum to acromium
• 2 finger widths down
• Feel the tubercle
• Drill into patient
• Use a YELLOW needle for servicemen

EZ-IO Insertion
IMPORTANT: Do NOT touch the needle set with your hands or fingers.
• Position the Driver at the insertion site with the needle at a 90 degree
angle to the bone.
• Push the needle through the skin until it is firmly against the bone ensuring
that at least one black line is visible above the skin prior to drilling.


IMPORTANT: Control the patient's movement prior to and during insertion.
• Penetrate the bone cortex by squeezing the Driver's trigger and applying
gentle, steady downward pressure.
• Release the Driver's trigger and stop when:
1. A sudden "give" or "pop" is felt upon entry into the medullary space.
2. The desired depth is obtained.
IMPORTANT: Use gentle-steady pressure. DO NOT USE EXCESSIVE FORCE.
Allow the needle set rotation and downward pressure to provide penetrating
action.
Note: If the Driver stalls and will not penetrate the bone, you may be applying too much
pressure.

• When the needle is seated correctly, unscrew the introducer and dispose of
the sharp.
• Attach the primed extension set to the EZ-IO catheter.
Do NOT attach a syringe directly to the EZ-IO catheter hub.

• Aspirate a small amount of marrow to confirm placement.
• Flush the EZ-IO catheter with 10mls of normal saline
Note: Frequently monitor the insertion site for extravasation.

To remove the catheter from the patient, attached a Luer-lock syringe,
continuously rotate clockwise which slowly and gently applying traction to
the catheter.
Do NOT rock or bend the catheter during removal.
• Dress the site as appropriate.
IV Fluids (Maintenance & Resuscitation)
History
Previous 24 hours fluid intake and excessive losses (eg. fever, diarrhoea, vomiting,
intensive exercise, environmental factors)
Examination
Can the patient tolerate oral fluids? (eg AVPU=AV, No GI injury, not vomiting)
Clinical monitoring should be performed routinely during and after fluid maintenance.
Record trends for HR, BP, RR, AVPU, volume and colour of urine, oral temperature,
blood glucose.
Management (basic)
Document your history and clinical findings then seek urgent advice from a medical
officer.
Work within your competency.
Give oral fluids where possible according to guidance below.
Management (advanced) – You must have completed the prolonged field care
course
Gain I/V or I/O access and follow guidance below.
Guidance:
1. Does the patient require emergency resuscitation fluids? If so, follow
the emergency resuscitation algorithm below in RED
Otherwise,
2. Oral hydration is the preferred option to maintain daily hydration otherwise
consider intravenous / intraosseous (IV/IO) fluid.
3. Total fluid intake for routine maintenance = 30ml/kg/day. Example 100kg = 3
Litres per day
4. Crystalloid (normal saline 0.9%) is the fluid of choice given at a rate of 100 -
150mls/hr. See chart for drip rate. 3L over 24 hours is approximately 42
drops per minute.
5. Passive leg raise above the level of the heart may be beneficial.


Cardiogenic Shock
Definition
• Cardiogenic shock is defined clinically as a poor cardiac output plus
evidense of tissue hypoxia that is not improved by correcting reduced
intravascular volume. When a pulmonary artery catheter is used,
cardiogenic shock may be defined as a cardiac index below 2.2L/minute/m²
despite an elevated pulmoary capillary wedge pressure (>15mmHg)
Aetiology
• Acute myocardial infarction is the most likely cause. Cardiogenic shock
occurs in about 7% of patients admitted with AMI and typically may be
present acutely or develop within 24-48 hours. Major risk factors for
developing cardiogenic shock with AMI are tachycardia or bradycardia,
hypotension, diabetes and previous MI.
Treatment
• Thrombolysis is unlikely to be beneficial in these cases and RCT has found
no signifcant difference in mortality at 21 days
• Medical supportive treatment can be provided with vasopressors, inotropes
and vasoconstrictors
• A large RCT has identified that early invasive cardiac revascularisation will
reduce mortality compared to medical treatment alone. This will require
judgement regarding the availability of local resources (Host Nation and/or
Neighbouring Nation) or the suitability for CCAST evacuation to Role 4
Neurogenic Shock
Definition
• Neurogenic shock is a form of "distributive shock" where loss of vascular
tone leads to a mal-distribution of blood flow
Aetiology and pathophysiology
• Injury to the spinal cord may interrupt the sympathetic chain resulting in
vasodilation with hypotension and warm peripheries. Symptoms are
more severe with high cervical cord lesions whereas lesions below T6
would rarely produce shock
• Loss of sympathetic innervation to the heart results in unopposed
parasympathetic activity with resultant bradycardia
• Patients who have lost sympathetic tone also lose some ability to
thermoregulate they do not sweat in the heat and they cannot
vasoconstrict in the cold
Treatment
• Beware attributing hypotension to spinal cord injury in the initial phases of
resuscitation: a patient with spinal cord injury may have warm extremities,
a bradycardia and a soft abdomen despite having a significant
haemoperitoneum. Presume hypotension is due to blood loss and
search for a source of bleeding (CXR, Pelvis, XR, FAST scan of
abdomen, CT clinical examination or long bones, catheter to exclude
haematuria from retroperitoneal bleed)
• Monitor the patients temperature: if the Resus Room is hot (desert
environment) be prepared to spray with water and fan to cool; if the room is
cold cover with blankets and use the hot air warming blanket.
• Use atropine for bradycardia
Go to Sepsis.
