Cervical Spine Trauma
Initial Assessment & Management
Immobilisation
Care under fire (CUF) and tactical field care (TFC)
• Care should be taken to keep head and neck movement to a minimum in this
phase of care BUT the operational need, control of catastrophic haemorrhage and
airway opening manoeuvres should not be compromised.
• Evacuation to a more secure area takes precedence over spinal immobilisation.
• Collars, scoop stretchers and head blocks should not be used in this phase of
care.
Permissive environment - Role 1
• A more detailed assessment can take place in this environment.
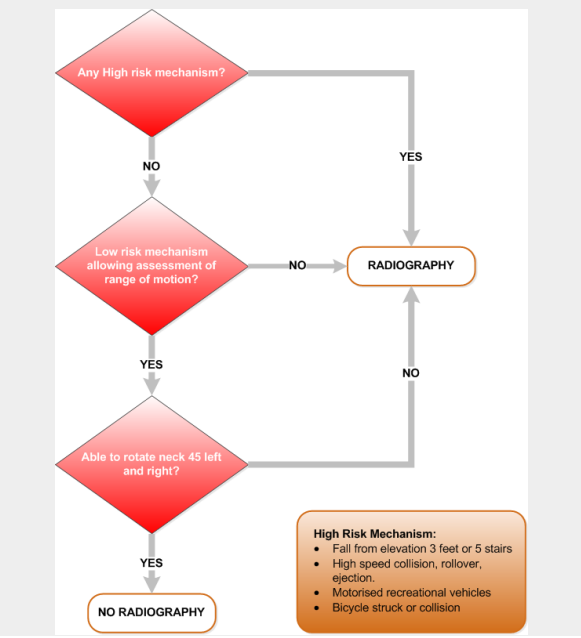
• It may be appropriate to apply the Canadian C-spine rules to help decide on the
appropriate management for a potential spinal injury.
• Methods of immobilisation chosen MUST take into account the time and method
of onward evacuation as the benefits must outweigh the risks of such interventions
(i.e. development of pressure areas, vomiting whilst immobilised).
• Patients who are unable to protect their own spine are in greater need of active
spinal precautions (i.e. those who are less than fully conscious and those who are
confused or combative).
• Adjuncts that may be used to immobilise a spine are cervical collar, head blocks
and tape or scoop stretcher and straps.
Points to note
• There is no role for a cervical collar following penetrating injury. A collar may
mask wounds and haematoma formation.
• The combative patient may not tolerate immobilisation in head blocks. To enforce
this may mean the head is pinned down while the rest of the body moves: this is not
desirable with a potential C-spine injury. Stabilise head and neck as best as possible
and continue to provide reassurance to the patient.
• Where there is concern for raised intracranial pressure (ICP) after a
closed head injury and the patient requires immobilisation, use only head
blocks and tape to secure the neck. If possible raise the head to 30
degrees and transfer the patient by helicopter with the head towards the
tail of the aircraft.
Advanced Assessment & Management
Log Roll
Examining the patient's back
• Traditionally a log roll has been a routine part of the primary survey in trauma. A
log roll is not always indicated and the risk of destabilising blood clot formation (i.e. in
pelvic fracture) may outweigh the benefit of a log roll.
• A log roll (or variant) must be undertaken, if penetrating injury is suspected.
• Rather than perform a 90 degree log roll, it may be more appropriate to undertake
a 15-30 degree trauma tilt to get a patient on a stretcher or scoop (i.e. undertake
minimum patient movement to attain the outcome required).
• The trauma tilt is ideally a 5 person technique (4 to undertake the manoeuvre
and 1 person to place the stretcher, administer dressings to the back etc).
Trauma tilt
• This technique would be used to remove clothing or body armour, place a
pelvic binder, remove any foreign bodies or place a scoop stretcher, warming
blanket or stretcher beneath the patient.
• A patient must never be placed on a spinal board (beyond initial extrication at
point of injury).
Log roll
• A 90 degree log roll may be required for assessment and management of
penetrating injuries to the back or buttock/perineal area.
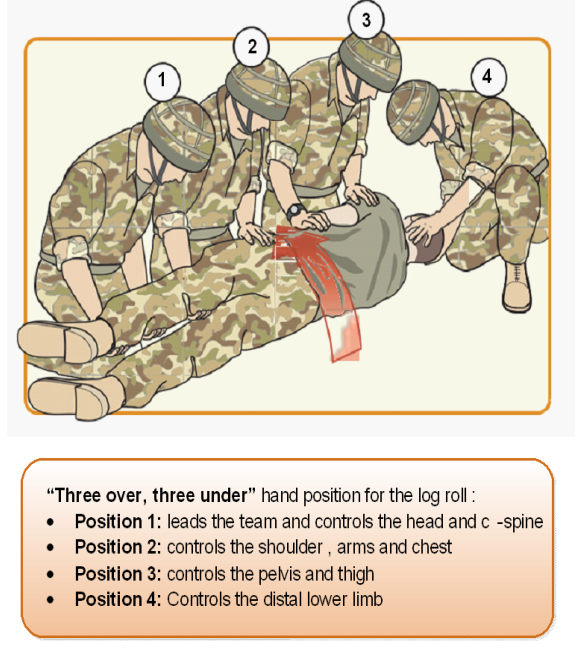
• The log roll is controlled by the clinician at the patient's head (team leader).
• Roll away from any injuries (i.e. if the patient has a left femur fracture, roll to
the patient's right).
• Ensure there is adequate slack in all lines (IV lines;ventilator tubing;
monitoring leads).
• Team leader uses the command "Ready-Brace-Roll" to ensure synchronous
movement when rolling onto the side. Consideration and direction to the degree
of roll to undertake must be assessed and communicated BEFORE any
movement.
• Palpation to the spine and/or a PR are not indicated in military PHEC. If there
is significant clinical concern to immobilise a patient, the patient should be
evacuated to a Role2+/R3 to have a CT scan.
• Once the necessary examination and interventions have taken place, the
team leader uses the command "Ready- Brace-Roll" to roll the patient onto their
back. Where the spine has not been radiologically and clinically cleared, the
cervical spine immobilsation is re-applied, if the patient requires it. If they are fully
alert and co-operative, they may be able to lie still without the need for the
discomfort of full immobilsation.
Spinal Clearance
NICE recommends the use of the Canadian Guidelines for C-Spine clearance. If in
doubt continue C-Spine immobilisation.
https://www.nice.org.uk/guidance/ng41
Airway Issues in C-Spine Injury
Indications for ventilation
Casualties with cervical cord injury above the level of C4 have diaphragmatic and
intercostal muscle paralysis and rely on accessory muscles for ventilation. They will
require early intubation to maintain adequate ventilation. Casualties with cord injury
between C4 and C8 retain the diaphragm function: however, loss of the intercostal
muscle function reduces the FVC and tidal volume by up to 60% and ventilatory support
may be required if the casualty tires.
